Abstract

Introduction: All patients with lower-risk (LR)-MDS experience primary or secondary failure of erythropoiesis-stimulating agents (ESAs), lenalidomide, or hypomethylating agents (HMAs), and there is an unmet need for other active therapies. IST has activity in patients with LR-MDS, but is infrequently used. We studied the clinical outcomes and predictors of response in patients with MDS treated with IST in a large multi-center international cohort.
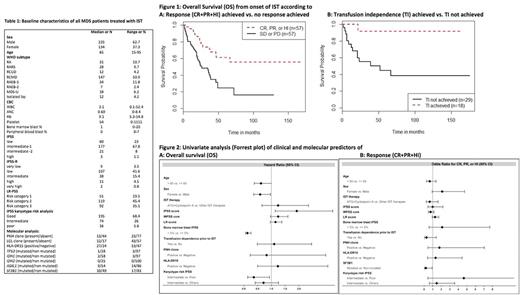
Methods: Data was collected from 11 centers in the United States and in Europe. Responses and red blood cell (RBC) transfusion independence (TI) were defined by the modified 2006 MDS IWG criteria. Kaplan-Meier methods estimated overall survival (OS) from initiation of IST to death or end of follow-up. Multivariable logistic regression models estimated odds for response and TI, and multivariable Cox Proportional Hazard models estimated hazards ratios (HR) for OS. Covariates included IST received, age at diagnosis, MDS classification, MDS risk category per International Prognostic scoring system (IPSS) and revised IPSS (IPSS-R), WHO-based Prognostic scoring system (WPSS), LR-MDS Prognostic Scoring System (LR-PSS), transfusion dependence, presence of paroxysmal nocturnal hemoglobinuria (PNH) and large granular lymphocytes (LGL) clones, HLA-DR15 positivity, IPSS-defined cytogenetic risk groups, and genetic mutations in TP53, IDH1/2, ASXL1 and SF3B1 genes.
Results: A total of 367 patients received IST; of these, disease risk according to the IPSS was low (23%), int-1 (68%), or either int-2 or high risk (9%). Median age at diagnosis was 65 years (range [R], 15-95), and 63% were male (Table 1). Median number of therapies prior to IST was 1 (R, 0-7) with 249 patients receiving ≥ 1 prior therapy. Most common prior therapies were ESAs (43%) and HMAs (29%). In 149 (40.6%) patients only prednisone was used; these patients were excluded from response and survival analysis. Of the other 198 patients, IST used from most to least frequently was ATG (46%: Rabbit/Horse 62/38%), cyclosporine (11%), tacrolimus (5%) and others (8%). ATG was combined with cyclosporine in 25% of patients. 114 of these 198 patients had response criteria reported: 13.2 % (95%CI, 7.8%-21.1%) had a complete remission (CR), 5.3% (95%CI, 2.2%- 11.6%), had a partial response (PR) and 31.6% (95%CI, 23.4%-41.0%) achieved hematologic improvement (HI) resulting in an overall response rate (ORR) of 45%. In contrast, 38.6% (95%CI, 29.8%-48.2%) of patients had stable disease (SD) and 11.4% (95%CI, 6.5%-19.1%) had progressive disease (PD). TI was achieved in 38.3% of patients. Median OS from time of IST initiation for all patients was 47.2 months (95%CI, 35-69.4 months). For patients who achieved a response (CR+PR+HI) to IST, the median OS was not reached (95%CI, 47 months-un-reached) whereas patients without a response had a median OS of 26 months (95%CI, 19.8-46.6 months) (p=0.0004) [Figure 1A]. Similarly, for patients who achieved TI with IST, median OS was not reached, whereas patients who remained transfusion dependent had a median OS of 52 months (95%CI, 20.7 months-un-reached) [Figure 1B]. In univariate analyses, female sex (female vs. male, HR 0.6, p=.04) predicted better OS whereas higher-risk IPSS (HR 1.9, p=.01) and IPSS-R score (HR1.3, p=.02) predicted worse OS [Figure 2A]. In multivariate analyses, only bone marrow blast >5% remained a statistically significant predictor of OS (>5% vs. ≤ 5%, HR 6.6, p<0.0001). In a univariate analysis of response, SF3B1 mutational status was associated with lower response rates (mutated vs. non-mutated, OR 0.2, p=.04); in multivariate analysis no predictive factors for response were identified. Importantly and in comparison to prior reports, age, prior transfusion dependence, MDS risk scores, type of IST used (ATG+cyclosporine vs. others), presence of a PNH or LGL clone and HLA DR15 positivity, and mutations were not predictive of response to IST [Figure 2B].
Conclusions: To our knowledge, this is largest reported cohort of patients with MDS treated with IST. While we confirmed that IST is associated with an ORR of 45% and leads to TI in 39% of patients, we could not confirm the predictive value of several previously described biomarkers of response. Apart from SF3B1 mutations, which appear to negatively affect response to IST, no other factors were identified that predicted response to IST. OS was better for patients who achieved an objective response or TI.
Sekeres: Celgene: Membership on an entity's Board of Directors or advisory committees. Brunner: Takeda: Research Funding; Celgene: Research Funding. Roboz: Cellectis: Research Funding; AbbVie, Agios, Amgen, Amphivena, Array Biopharma Inc., Astex, AstraZeneca, Celator, Celgene, Clovis Oncology, CTI BioPharma, Genoptix, Immune Pharmaceuticals, Janssen Pharmaceuticals, Juno, MedImmune, MEI Pharma, Novartis, Onconova, Pfizer, Roche Pharmace: Consultancy. Steensma: Pfizer: Consultancy; Takeda: Consultancy; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Research Funding; Incyte: Equity Ownership; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy; Onconova: Consultancy; H3 Biosciences: Consultancy. Platzbecker: Acceleron: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Research Funding; Celgene: Consultancy, Honoraria, Research Funding. Fenaux: Janssen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Astex: Honoraria, Research Funding; Astex: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Amgen: Honoraria, Research Funding. Fathi: Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria; Seattle Genetics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Juno: Membership on an entity's Board of Directors or advisory committees; Medimmune: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Research Funding; Agios: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Germing: Novartis: Honoraria, Research Funding; Janssen: Honoraria; Celgene: Honoraria, Research Funding. Ritchie: Bristol-Myers Squibb: Other: Research funding to my institution; Astellas Pharma: Other: Research funding to my institution; Celgene: Consultancy, Other: Travel, Speakers Bureau; Incyte: Consultancy, Speakers Bureau; Pfizer: Consultancy, Other: Research funding to my institution; NS Pharma: Other: Research funding to my institution; Novartis: Consultancy, Other: Research funding to my institution, and travel, Speakers Bureau. Podoltsev: Incyte: Consultancy; Alexion: Consultancy; Ariad: Consultancy; CTI biopharma/Baxalta: Consultancy. Santini: Janssen: Consultancy, Honoraria; Amgen: Membership on an entity's Board of Directors or advisory committees; Otsuka: Consultancy; Novartis: Honoraria; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Research Funding. Komrokji: Novartis: Honoraria, Speakers Bureau; Celgene: Honoraria. Zeidan: Otsuka: Consultancy; Takeda: Speakers Bureau; AbbVie, Otsuka, Pfizer, Gilead, Celgene, Ariad, Incyte: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract